|
Departments of Developmental Therapeutics and Biomathematics.
The University of Texas System Cancer Center M.D. Anderson Hospital
and Tumor Institute. 6723 Bertner, Houston, Texas 77030 USA
Supported in part by Grants CA 11520. CA05831. CA 19806 and CA 14528.
National Institutes 01f Health. Bethesda. Maryland.
The introduction of combination chemotherapy in the treatment of
adult acute leukemia has had a profound impact on the response and
duration of survival of patients with adult acute myeloblastic leukemia.
In the past decade. the combination ofcytosine arabinoside with
an anthracycline antibiotic. either daunorubicin. adriamycin, or
rubidazone, has been responsible to a large degree for the success.
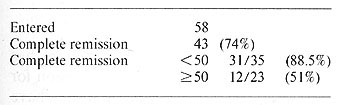
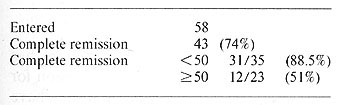
In a study done at the M. D. Anderson Hospital in 1973, a combination
of adriamycin. vincristine. Ara-C and prednisone (Table 1) was utilized
for initial induction therapy for 58 adults between the age of 15
and 76 with a diagnosis of acute myeloblastic leukemia. 43 (74%
) of the patients achieved a complete remission with 31 of 35 (89%)
patients under the age of 50 achieving a complete remission [4].
Median duration of survival in this group of patients was 58 weeks.
Nine patients remain alive between 4 and 5 years from diagnosis.
These 9 are all in their original first complete remission and represents
9 of 31 Patients (29% ) under the age of 50 who achieved remission.
Table 1. AD-oap. Acute myeloblastic leukemia
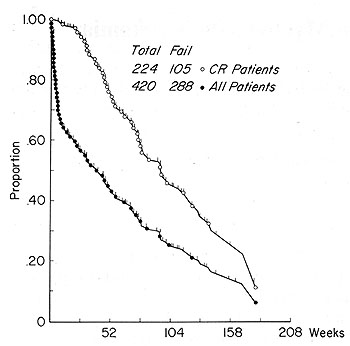
Because of the initial success of this program, the same combination of agents was utilized in the Southwest Oncology Group for remission induction therapy. A total of 420 patients were entered, 224 achieved complete remission (54%). The survival of all patients and survival of those patients achieving a complete remission is shown in Fig. I. The vertical lines on these survival curves represent patients still alive and can still effect the overall survival of these patients. The median duration of survival of all patients entered is 50 weeks and the projected median duration of survival of the patients who achieved complete remission is almost double this to 2 years [5].
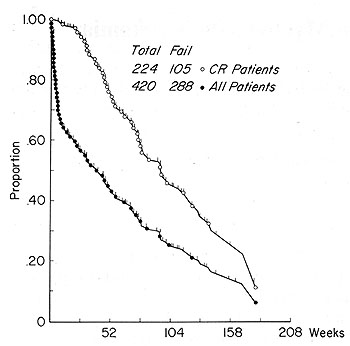
Fig. 1. Swog 7416/17. Acute myeloblastic Ieukemia survival
from first treatment
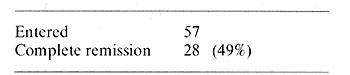
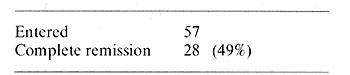
In addition to adriamycin, rubidazone, a new anthracycline antibiotic
related to daunorubicin, has been utilized in combination with cytosine
arabinoside in the management of patients over the age of 50. The
program is shown in Table 2. A total of 56 patients have been entered
on this program with an overall response rate of 49% which is similar
to the response rate seen in patients utilizing a combination of
adriamycin, Ara-C, vincristine and prednisone [3].
Table 2. Roap. Acute myeloblastic leukemia.
>50 years of age
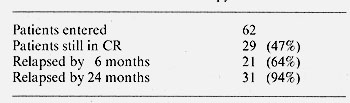
In an attempt to prolong remission, a late intensification program
has been used in patients who have been in maintained complete remission
for one year or longer. Late intensification therapy utilizes drugs
that they have not been previously exposed to, the majority of the
patients in this program received a combination of 6-mercaptopurine,
methotrexate, vincristine and prednisone. A total of 62 patients
have undergone late intensification therapy and 29 ( 47% ) remain
in unmaintained complete remission. The majority of the patients
that relapsed, relapsed in the first six months and 31 of the 33
patients that have relapsed have done so within the first 24 months
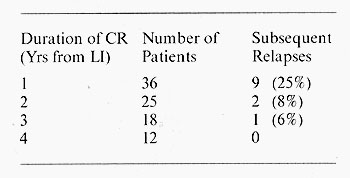
following discontinuous of chemotherapy (Table 3). The risk of relapse
sub
Table 3. Late intensification therapy
in acute leukaemia
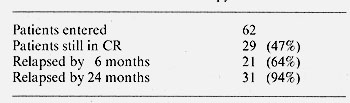
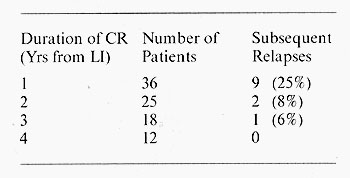
sequent to this time is less than 10% [ 1]. Of the 36 patients who
are in continuous complete remission one year from complete remission.
9 (25% ) had relapsed whereas 12 patients now have been discontinued
from chemotherapy four years or longer from the late intensification
and none of these have relapsed (Table 4). The overall risk of subsequent
relapse after one year of continuous complete remission without
chemotherapy is less than 10%.
Table 4. Duration of unmaintained remission
alter late intensification therapy
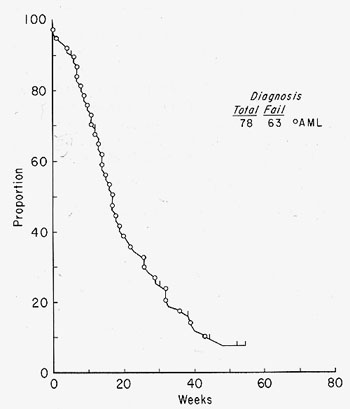
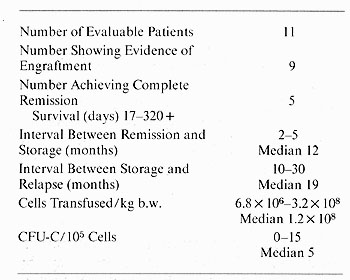
The survival in AML after relapse is short. the median duration of survival of patients with AML who have achieved a complete remission and subsequently relapsed. the survival from relapse is less than 20 weeks (Fig. 2). Only 5% of these patients are projected to be alive in one year. Because of these poor results following relapse. a program of autologous bone marrow transplantation has been introduced using marrow collected and stored from patients with acute myeloblastic leukemia during periods of remission. This therapy offers a viable alternative to reinduction chemotherapy . We have used a combination of piperazinedione and total body irradiation therapy.
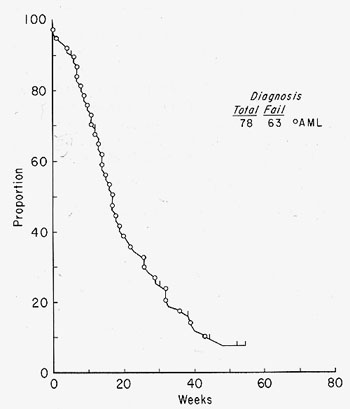
Fig.2. Survival from relapse
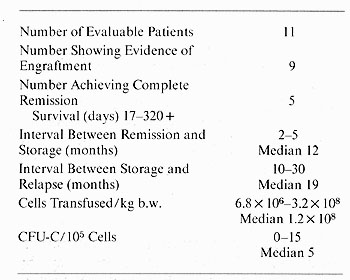
This program has resulted in clearing of the leukemia and evidence
of engraftment with normal myeloid recovery in 5 of II patients
[2]. Survival of these patients. duration of remission and duration
of bone marrow storage in months and interval between storage and
relapse and the number of cells and the number of colony forming
units reinfused is shown in Table 5.
Table 5. Autologous bone marrow transplantation
References
1. Bodev. G. P.. Freireich. E. .1.. McCredie. K. B.. Rodriguez.
V.. Gutterman. .1. U.. Burgess II. M.A.: Late intensification chemotherapy
for patients with acute leukemia in remission JAMA 235, 1021-1025
( 1975)
2. Dicke. K. A.. McCredie. K. B.. Stevens. E. E.. Spitzer. G.. Bottino.
J. C.: Autologous bone marrow transplantation in a case of acute
adult leukemia. Transplant. Proc. 9, 193-195 (1977)
3. Keating. M.J.. Benjamin. R.S.. McCredie. K.B.. Bodey. G.P.. Freireich.
E.J.: Remission induction therapy with a rubidazone-containing combination
(ROAP) in acute Ieukemia. P. 180. Proceedings of the 68. Annual
Meeting ofAACR/ ASCO. 1977. Abstract No.719 '
4. McCredie. K. B.. Freireich. E..I.: Acute leukemia: Chemotherapy
and Management. In: Clinical cancer chemotherapy. Greenspan. E.
M. (ed.). pp. 71-109. New York: Raven Press 1975
5. McCredie. K. B.. Hewlett. J. S.. Gehan. E. A.. Freireich. E.J.:
Chemoimmunotherapy of adult acute leukemia (CIAL). p. 127. Proceedings
of the 68. Annual Meeting of the AACR/ ASCO. 1977. Abstract No.506
|