|
Hematologie-Oncology and Radiotherapy Services,
St. Jude Chrildren's Research Hospital, Memphis, Tennessee 38101.
Supported by Cancer Research Center Grant CA-O8480, Research Project
Grants CA07594 and CA-13050, and Training Grants CA-05176 and CA-08151
from the National Institutes of Health, by Project Grant CI-70 from
the American Cancer Society and by ALSAC.
Introduction
The gratifying results now being obtained in the treatment of children
with acute lymphocytic leukemia has had at least two major effects
on the attitude of the medical community. First, these results have
encouraged physicians to think of ALL as an eminentably treatable
and, perhaps, curable disease, Second, physicians have become more
aware of the obligation to avoid serious side effects that might
compromise the otherwise good results. My purpose in speaking to
you today is to review briefly some of the results obtained, mainly
at our own institution, in the treatment of this disease and to
point out some of the problems that have been encountered as result
of treatment. Our data has been reported in some detail recently
(19) so I will present only selected points rather than an exhausive
review. Some of the results I will talk about today are preliminary
and will require months or years before definitive conclusions can
be made.
Materials and Methods
Definitions
Acute lymphocytic leukemia (ALL) is diagnosed on the basis of excessive
numbers of lymphoblasts and/or "stem cells" in an aspirated bone
marrow specimen. In practice, this diagnosis includes all children
with leukemia that is not characterized by Auer rods or myelocytic
or monocytic differentiation. Special cytochemical stains and histological
specimens are sometimes helpful, but, ultimately, the diagnosis
ist the concensus of at least three experienced investigators. Approximately
78 0/0 of leukemia cases at this institution are diagnosed as ALL.
Children with lymphoblastic or "stem cell" lymphosarcoma who had
marrow involvement at diagnosis are considered to have ALL and are
included in these studies. Our definitions of remission, relapse
and survival are described in detail elsewhere (15 ). Complete remission
duration is the period free of all signs of ALL, whether hematologic,
visceral or in the CNS. CNS leukemia is diagnosed by the observation
of leukemia cells in a Wright-stained centrifugate of cerebrospinal
fluid (CSF). The appearance of leukemia cells in the bone marrow
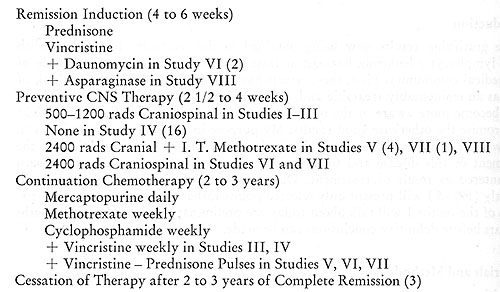
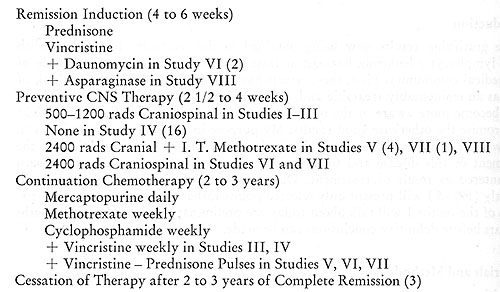
signifies hematologic relapse. Methods A brief outline of the treatment
plan for the first seven studies is shown in Table 1. This shows
some of the variations on the theme of therapy that has been used
over the years. Basically however, treatment entails four phases:
1) remission induction, 2) preventive CNS therapy , 3) continuation
( maintenance) chemotherapy, and 4) cessation of therapy.
Table I: Outline of Protocols
Patients
These studies include a total of 549 children with ALL, of whom
363 entered studies I through VII, from 1962 through 1971. From
1972 to the present, 186 previously untreated children have entered
study number VIII which is still under way. The initial features
of a majority of these patients have been reported elsewhere (19).
Results
Remission Induction
Successful remission induction has been obtained in over 90 % of
children with ALL. Vincristine and prednisone has been the treatment
used in most of these studies and the addition of daunorubicin or
asparaginase has not appreciably improved the remission induction
rate. The reason for failure of patients to attain complete remission
include: fatal infection in 2.5 %, usually due to gram-negative
sepsis ill the first week of therapy; failure to respond to chemotherapy
in 5 %; and leukemic pleocytosis in the cerebral spinal fluid on
the day of first complete remission marrow in 1 %.
Preventive Central Nervous System Therapy
Attempts were made in earlier studies to prevent CNS leukemia from
emerging by eradiating undetectable cells in the meninges early
in remission. These early studies employed 500 or 1200 rads of craniospinal
irradiation. However, these doses of irradiation did not reduce
the frequency of CNS leukemia which terminated complete remission
in 15 of 37 patients (18). In 1967 it was decided that failure to
prevent CNS leukemia in the earlier studies may have been due to
inadequate dosage. Therefore, a study was designed in which 2400
rads of cranial radiation was given along with 5 doses of intrathecal
methotrexate simultaneously ( 4 ). This form of treatment met with
success since CNS leukemia terminated complete remission in only
3 of the 37 patients (19). Furthermore, over one-half of these patients
remain in initial continuous complete remission for 6 years and
have been off all therapy for three years. The efficacy of preventive
CNS irradiation was tested in a randomized control study before
the results of the previous study were known (2). Patients were
randomized to receive or not to receive 2400 rads craniospinal irradiation
without intrathecal methotrexate. CNS leukemia terminated complete
remission in only 2 of 45 patients who received preventive irradiation.
However, CNS leukemia terminated complete remission in 33 of 49
patients who did not receive preventive irradiation. This study
provided further evidence that CNS leukemia could indeed be prevented
with adequate doses of irradiation. Another feature of this study
was to determine whether CNS irradiation at the same dosage level
would be as effective if given at the first sign of CNS relapse.
Therefore, the 33 patients who developed CNS leukemia were given
therapeutic craniospinal irradiation. Although the CSF was cleared
of leukemic cells in all 33 patients, this second complete remission
was terminated by recurrence of CNS leukemia in 13 patients and
by simultaneous hematological and CNS relapse in 2. Only 9 of the
33 have had a lengthy second complete remission. In a subsequent
study, patients were randomized to receive either 2400 rads cranial
irradiation with simultaneous intrathecal methotrexate or 2400 rads
craniospinal irradiation (1). The results showed no significant
difference between in the rate of CNS relapse with either form of
therapy, which confirmed the historical controls of the two preceding
studies.
Continuation ( Maintenance ) Chemotherapy.
In the above studies, patients received mercaptopurine daily and
methotexate and cyclophosphamide weekly during the continuation
phase of chemotherapy. A controlled study (16) has shown that these
agents must be given in maximum tolerated dosage to achieve optimal
results. Variations on this basic regimen have included the addition
of vincristine once a week or periodic brief courses of rincristine
plus prednisone. With the overall improvement in results, it became
important to try to learn the relative contribution of CNS therapy
and continuation chemotherapy. The earlier studies, with apparently
ineffective CNS therapy, had yielded a 17% longterm leukemia-free
survival rate. This had been improved to approximately 50 % in the
studies using the higher dose of preventive CNS irradiation (19).
In view of the major contribution of adequate CNS therapy, it was
not known whether such aggressive chemotherapy during remission
was necessary in view of its toxicity with a disturbing proportion
of patients dying during initial continuous complete remission (21).
An attempt to improve the therapeutic index of continuation chemotherapy
by reducing toxicity was the major purpose behind the design of
Total Therapy Study VIII. The preliminary results of this study
are given here with the understanding that they are not definitive
at this point, but do yield some important observations even at
this early date. The principal goal of Study VIII is to learn how
the therapeutic index of chemotherapy during remission might be
improved. Combination chemotherapy has been used to take advantage
of different modes of action and lack of cross-resistance. The value
of combination chemotherapy for inducing remission was established
in 1951 with cortisone and methotrexate ( 6) and subsequently for
other combinations (7, 8). Combinations of two or more drugs have
also been given for continuing remission. For example, most of our
studies employed a combination of mercaptopurine, methotrexate,
and cyclophosphamide. There have been controlled studies of the
cyclic (rotation of several drugs, one at a rime) versus sequential
(single drugs, each until relapse) chemotherapy (5, 12) and of the
addition of one or another drug to a basic regimen (13 ). Controlled
studies of different drug combinations began with the classical
study by Acute Leukemia Group B (7a). The first controlled study
of single versus combination chemotherapy, also performed by Group
B, later showed that median durations of remission in childhood
ALL were the same with mercatopurine, methotrexate, or both agents
given simultaneously in the same dosages as in the single drug regimes
(7). Since then, improved remission durations have been obtained
in some studies using multipledrug therapy (8, 20) leading to increasingly
complex, mu]tiple-drug regimens. For example, the L-2 protocol from
Memorial Hospital employs eight drugs in cycles designed to take
maximum advantage of estimated cellular kinetics (9). However, individual
drugs are not equally effective for prolonging remission of childhood
ALL (8). Intermittent methotrexate is better than mercaptopurine
and either is better than cyclophosphamide. Vincristine, cytosine
arabinoside, daunomycin, asparaginase and other agents apparently
are less effective. Most of these agents have overlapping toxicity,
particularly myelosuppression and immunosuppression, often lowering
the tolerable dosage limits of each drug in a multiple-drug regimen.
In any given schedule, the effectiveness of single (8) or multiple
(16) drugs is related to dosage. Thus, the critical question emerges:
Does the advantage of multiple agent chemotherapy outweigh the disadvantage
of dosage reduction of the more effective agents? An affirmative
answer could lead one to employ all available agents (as many as
six or ten) while a negative answer could lead to use of only the
most effective agent (methotrexate) in maximum-tolerated dosage.
Study VIII was designed to answer this question. After successful
remission induction and preventive CNS therapy, patients are randomized
to receive one, two, three, or four drugs simultaneously during
remission. The prescribed dosages are starting points only and in
each regimen drug dosages are adjusted to the maximum tolerated
by the patient. Upward or downward dosage adjustments are made proportionately
for all prescribed drugs. To obtain valid conclusions it is essential
that the dose-Iimiting toxicity be of comparable degrees in each
group to avoid the "half-dosage effect" seen in Study IV (16). The
principal guide for dosage for dosage adjustment ist maintenance
of the leukocyte count between 2000 and 3500/mm³. Dosage reductions
allowed for other predetermined degrees of toxicity, fever or infection
are the same for all groups. The preliminary results of Study VIII
are given here mainly to illustrate the points of rationale and
must not be viewed as conclusive at this early date. In the 33 months
since beginning this study, 180 patients attained complete remission
and received preventive CNS therapy. Thirty were given additional
initial therapy due to the presence of features (CNS involved at
diagnosis, mediastinal involvement, failure to attain remission
after 4 weeks) associated with a poor prognosis and were not randomized.
All received three drug maintenance. The remaining 150 were randomized
to receive (1) methotrexate alone; (2) methotrexate + mercaptopurine;
(3) methotrexate + mercaptopurine + cyclophosphamide; (4) methotrexate
+ mercaptopurine + cyclophosphamide + cytosine arabinoside. All
agents except merca ptopurine were gi ven by vein weekl y . At this
time, the frequency of relapse has been approximately the same among
patients receiving two drugs (6 of 44), three drugs (10 of 45) or
four drugs (3 of 41 plus two deaths in remission). With methotrexate
alone, 14 of 20 have relapsed and one patient died in initial remission.
These early results show no systematic assocation of efficacy with
the number of drugs but apparently indicate the superiority of multiple
agents over methotrexate alone. The smaller number of patients in
the group receiving methotrexate alone is the result of discontinuing
randomization to that arm of the study. This action was taken because
the relapse rate was higher but, more importantly, a serious side
effect was observed in this group. Eight of the twenty patients
developed a neurological syndrome, not associated with CNS leukemia.
It was characterized by disturbances of gait, speech and motor function.
This syndrome was progressive and fatal in one child and left permanent
residual damage in several others. The pathological lesion was found
to be a severe leukoencepholopathy with myelin degeneration. This
syndrome usually occurred in patients who had been receiving more
than 50 mg per meter squared of methotrexate weekly for 6 months
or more. A more detailed analysis of this problem is underway and
will be reported in the near future. For the time being however,
no patient who has received brain irradiation will be given more
than 50 mg per meter squared per week of methotrexate by vein at
this institution. This observation should serve to caution other
investigators who are giving high doses of methotrexate to patients
who had CNS , irradiation.
Discussion
The efficacy and dangers of combined modality therapy of childhood
ALL arc reflected in these studies. The search by many investigative
groups for more effective and less toxic modalities and combinations
of therapy is illustrated by the scope of a few current studies.
A recent Medical Research Council Study (28) has shown that CNS
leukemia is effectively prevented by craniospinal irradiation with
intrathecal methotrexate. A review of previous trials (25) and the
anatomical nature of arachnoid leukemia (31) have led us to conclude
that intrathecal methotrexate alone does not effectively prevent
CNS leukemia. However, studies by Group B (10) and the Sothwest
Oncology Group now in progress, as well as the L-2 Protocol at Memorial
Hospital (9), should yield more information on the preventive valu~
of intrathecal methotrexate. Since systemic chemotherapy in maximum-tolerated
dosage delayed the onset of CNS leukemia in Study IV (11, 15, 16),
the definitive results with even more aggressive systemic chemotherapy
in the L-2 Protocol (9) will be of interest. Another approach under
study by Children's Cancer Study Group A is a test of the value
of extending irradiation of the CNS to include other organs such
as liver, spleen, kidneys and gonads. The question of when to stop
therapy is an important one. It has been our practice to stop therapy
after two to three years of complete remission. Our experience with
this approach has been published recently (3 ). Despite improvement
in therapy, many old problems remain unsolved and new problems have
emerged. Both patient and physician take little satisfaction in
a longer survival unless it is of satisfactory quality, but, we
must remind ourselves that the most important negative influence
on quality of survival is the leukemia itself. By any standard of
comparison, the cost of relapse and its complications in human and
monetary resources far exceeds that of therapy. Nonetheless, the
evolution of studies for childhood ALL demonstrates a keen awareness
of the responsibility to minimize undesirable effects of therapy.
This requires even more careful design of studies because with combined
modality therapy, the side effects may not be due to a single agent
but to the unfortunate synergism of several agents.
References
1. Aur, R. J. A., Hustu, H. 0., Verzosa, M. S., Wood, A., and
Simone, J. V.: Comparison of two methods of preventing central nervous
system leukemia. Blood 42: 349-357,1973.
2. Aur, R. J. A., Simone, J. V., Hustu, H. 0., and Verzosa, M. S.:
A comparative study of central nervous ystem irradiation and intensive
chemotherapy early in remission of childhood acute lymphocytic leukemia.
Cancer 29: 381-391, 1972.
3. Aur, R. J. A., Simone, J. V., Hustu, 0., Verzosa, M. S., and
Pinkel, D.: Cessation of therapy during complete remission of childhood
acute lymphocytic leukemia. New Eng. J. Med. 291: 1230-1234,1974.
4. Aur, R. J. A., Simone, J., Hustu, H. 0., WaIters, T., Borells,
L., Pratt, C., and Pinkel, D. : Central nervous system therapy and
combination chemotherapy of childhood lymphocytic leukemia. Blood
37:272-281,1971.
5. Colebatch, J. H., Baikie, A. G., Clark, A. C. L., Jones, D. L.,
Lee, C. W. G., Lewis, I. C., and Newman, N. M.: Cyclic drug regimen
for acute childhood leukemia. Lancet 1: 313-318,1968.
6. Farber, S., Toch, R., Sears, E. M., and Pinkel, D.: Advances
in chemotherapy of cancer in man. Advances Cancer Res. 4: 1-22,
1956.
7. Frei, E., III, Freireich, E. J., Gehan, E., Pinkel, D., Holland,
J. F., et al.: Studies of sequential and combination antimetabolite
therapy in acute leukemia: 6-mercaptopurine and methotexate, from
the Acute Leukemia Group B. Blood 18: 431-454,1961.
7a. Frei, E., III, Holland, J. F., Schneiderman, M. A., Pinkel,
D., Selkirk, G., Freireich, E. J., Silver, R. T., Gold, G. L., and
Regelson, W.: A comparative study of two regimens of combination
chemotherapy in acute leukemia. Blood 13: 1126,1958.
8. Goldin, A., Sandberg, J. S., Henderson, E. S., Newman, J. W.,
Frei, E. III, and Holland, J. F. : The chemotherapy of human and
animal acute leukemia. Cancer Chemother. Rep. 55: 309-507,1971.
9. Hagbin, M., Tan, C. C., Clarkson, B. D., Mike, V., Burchenal,
J. H., and Murphy, M. L.: Intensive chemotherapy in children with
acute lymphoblastic leukemia (L-2 Protocol). Cancer 33: 1491-1498,1974.
10. Holland, J. F., and Glidewell, 0. : Chemotherapy of acute lymphocytic
leu kemia of childhood. Cancer 30:1480-; 1487,1972.
11. Hustu, H. 0., Aur, R. J. A., Verzosa, M. S., Simone, J. V.,
and Pinkel, D.: Prevention of central nervous system leukemia by
irradiation. Cancer 32: 585 597,1973.
12. Krivit, W., Brubaker, C., Thatcher, L. G., Pierce, M., Perrin,
E., and Hart mann, J. R.: Maintenance therapy in acute leukemia
of childhood: Compari son of cyclic vs. sequential methods. Cancer
21: 352-356, 1968.
13. Leikin, S., Brubaker, C., Hartmann, J., Murphy, M. L., and Wolff,
J.: The use of combination therapy in leukemia remission. Cancer
24: 427-432, 1969.
14. Medical Research Council: Treatment of acute lymphoblastic leukaemia:
Ef fect of "prophylactic" therapy against central nervous system
leukaemia. Brit. Med. J. 2: 381-384,1973.
15. Pinkel, D.: Five-year follow-up of "total therapy" of childhood
lymphocytic leukemia. J.A.M.A. 216: 648-652,1971.
16. Pinkel, D., Hernandez, K., Borella, L., Holton, C., Aur, R.,
Samoy, G., and Pratt, C. : Drug dosage and remission duration in
childhood lymphocytic leukemia. Cancer 27: 247-256, 1971.
17. Price, R. A., and Johnson, W. W.: The central nervous system
in childhood lymphocytic leukemia. I. The arachnoid. Cancer 31:
520-533, 1973.
18. Simone, J. V.: Treatment of children with acute lymphocytic
leukemia. Advan. Pediat. 19: 13-45,1972.
19. Simone, J.: Acute lymphocytic leukemia in childhood. Sem. Hemat.
11: 25 39, 1974.
20. Simone, J. V.: Aur, R. J. A., Hustu, H. 0., and Pinkel, D.:
"Total Therapy" studies of acute lymphocytic leukemia in children.
Current results and pros pects for cur. Cancer 30: 1488-1494,1972.
21. Simone, J. V., Holland, E., and Johnson, w.: Fatalities during
remission of childhood leukemia. Blood 39: 759-770, 1972.
|