|
G-CSF with Autologous Marrow Transplantation
Recombinant growth factors are being tested intensively in order
to modify the hematopoietic toxicity of high-dose therapies associated
with protracted absolute neutropenia. High-dose cyclophosphamide
(Cytoxan) 6 mg/m², carmustine (BCNU) 300 mg/m², and etoposide (VP-16)
750 mg/m² (CBV therapy) with autologous bone marrow transplantation
(ABMT) has been shown to be very effective therapy in relapsed Hodgkin's
disease [3, 4, 7]. Complete response (CR) was achieved in 45% of
the patients, 75 %) of these enduring on to more than 5 years. The
major toxicity of this potentially curative therapy is related to
fevers and infections during the neutropenic phase. Most patients
(>90 %) ) suffer from febrile episodes during the period of neutropenia,
approximately one-quarter of patients have clinical symptoms or
radiological changes consistent with pneumonia, a third or more
documented bacteremia, and approximately one-quarter suffered from
severe mucositis [3, 4]. CBV therapy is an important high-dose therapy
to study the impact of recombinant growth factors on toxicity. In
our first study we selected G-CSF because of its relatively restricted
proliferative action to neutrophilic granulocytes alone, without
any known in vivo induction of eosinophilia. We initially performed
a phase II study employing G-CSF by a 30 minute blous infusion at
a dose of 60 µ/kg per day beginning 24 h after marrow reinfusion
in 18 patients with Hodgkin's disease who received CBV therapy [9,
101 and sequently by continuous infusion over a range of doses,
including even greater doses in another 21 patients.
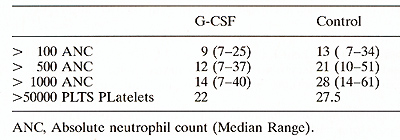
Table 1. Haematopoietic recovery: bolus
infusion
From Table 1 it is obvious that the difference in recovery to an
absolute neutrophil count (ANC) of 1000/µ1 is remarkably faster,
14 days, with G-CSF than control patients. Recovery to 500 ANC is
impressive, 9 days faster, but to lOO ANC recovery is only 4 days
faster. These patterns of recovery are identical to the best recoveries
of other studies using either G, or GM-CSF after autologous marrow
transplantation [1,5] .However, the febrile episodes were not significantly
decreased and days febrile marginally different. There is a drop
to below 100/µ1 ANC on days 8-10 following the initiation
of chemotherapy, 2 days after ABM infusion and arise to > 100/µ1
neutrophils on days 19-21 after chemotherapy. Therefore, despite
use of recombinant growth factors there is still an absolute neutropenic
period ( <lOO neutrophils/µl) of approximately 7-10 days.
Toxicity is related to complications occurring during the absolute
neutropenic interval. The frequency of febrile episodes in patients
receiving G-CSF remains unchanged (95 % ) .The onset of fever frequently
(95% ) occurs during the first 5- 7 days of absolute neutropenia.
Recombinant growth factors hasten neutrophil recovery over that
of ABM alone. But, growth factor accelerates predominately the terminal
part of neutrophil recovery and this is not necessarily enough to
modify the
morbidity, mortality or cost of ABMT in the majority of patients.
There continues to be approximately 7 days of absolute
neutropenia ( < 100/µ1) even with growth factor support.
The difference in neutrophil emergence in the tissues and saliva
between controls and growth factor treated patients may be even
less than the 4 days difference to lOO granulocytes.
Growth Factor-Mobilized Peripheral Blood Cells and the Absolute
Neutropenia
To enhance recovery even further we and others have proposed that
it is probably necessary to infuse significantly higher numbers
of progenitor cells [2, 11] .However, does peripheral blood really
enhance neutrophil recovery over that achievable with the use of
ABM alone or ABM with recombinant growth factor? Studies reported
by us in abstract form and to be published suggest that neutrophil
recovery is not improved compared to either our data with G-CSF
and ABM or those of other studies using GM-CSF. The clinical study
that we refer to evaluated the effects of peripheral blood stem
cells collected following chemotherapy and GM-CSF and added to ABM
and GM-CSF. The major question was does the addition of peripheral
blood collected in such a fashion and added to ABM and GM-CSF further
diminish the duration of neutropenia? To optimize the collection
of peripheral blood we followed the basic concept of Gianna et al.
[2]. Patients received a priming dose of doxorubicin 50 mg/m² by
continuous infusion (CI) over 48 hand cyclophosphamide 3 g/m² IVon
day 1. On day 4, they were started an GM-CSF by Clover four hours
at 0.6 mg/m² per day, which continued if tolerated through day 18
or until white blood cell count (WBC) reached 20 000, at which time
the dose was halved (0.3,0.15, and 0.075 mg/m² per day) each day
as long as the WBC count was < 20000/µ1. On day 18, all GM-CSF was
ceased. Peripheral stem cell storage by apheresis was performed
on consecutive weekdays until a minimum of 4 times 10high 8 mononuclear
cells/kg had been collected. After marrow and peripheral blood stroage,
the patients then received CVP in the doses described below. We
administered two courses of high-dose therapy. For each course of
therapy we administered cyclophosphamide 1.5 gm/m² per day times
3 (days 1-3), etoposide (VP-16) 400 mg/m² per day times 3 (days
1-3), and cisplatinum 55 mg/m² per day times 3 (days 1-3). On the
fifth day ofeach cycle of CVP, patients received GM-CSF at a dose
of 0.6 mg/m² as a 4-h IV infusion until an absolute neutrophil count
of 1500 µI was maintained for 2 consecutive days. The dose was halved
daily till the absolute neutrophils remained >1000. If absolute
neutrophils fell below 1000 during the tapering off of GM-CSF, the
dose was doubled daily until absolute neutrophils were >1000 for
two consecutive days at which time they were tapered as described
above. On the sixth day of cycle 1 CVp, one-half of the stored bone
marrow was infused. On the sixth day of cycle 2 CVP, the remaining
half of the bone marrow plus all the peripheral blood stem cells
were infused. Patients received a second cycle of therapy commencing
as soon as hematologic recovery had occurred ( defined as granulocyte
count > 1000/µ1 and platelet count >lOO OOO/µI), and reversible
non-hematologic toxicity had returned to baseline. Distinct from
other studies patients were not isolated. In this way the contribution
of peripheral blood to hematopoietic recovery over that of marrow
and GM-CSF alone could be determined.We concluded that peripheral
blood infusion did not enhance granulocyte recovery, or reduce febrile
episodes, days febrile or documented infections. However, there
was a reduction in the numer of platelet transfusions during the
second cycle (from five to two) and enhanced early platelet recovery
(11) .
Conclusions
Recombinant growth factors following transfusion of ABM and/or
peripheral blood cells apheresed following recombinant growth factors
with or without preceding chemotherapy have contributed in modest
ways to hematopoietic recovery. Patients with exceptionally prolonged
recovery following marrow infusion may benefit the most from addition
of peripheral blood cells. Peripheral blood collected during the
early phase of recovery from cytotoxic chemotherapy with high-numbers
of colony-forming units-granulocyte/macrophage (CFU-GM) does cause
earlier neutrophil recovery than ABM but is not necessarily faster
than ABM with recombinant growth factor. Platelet recovery is enhanced.
However, these are highly selected patients and the ability to enhance
recovery in heavily pretreated patients not necessarily proven.
Efforts to develop more effective methods to further enhance hematopoietic
recovery are still needed.
References
I. Brandt SJ, Peters Wp, Atwater SK, Kurtzberg J, Borowitz MJ,
lones RB, Shpall EJ, Bast RC, Gilbert CJ, Oette OH (1988) Effect
of recombinant human granulocyte macrophage colony-stimulating factor
on hematopoietic reconstitution after high-dose chemotherapy and
autologous bone marrow transplantation. N Engl J Med 318:869-876
2. Gianni AM, Bregni M, Stern AK, Siena S, Tarella C, Pileri A,
Bonadonna G (1989) Granulocyte-macrophage colony-stimulating factor
to harvest circulating hematopoietic stem cells for autotransplantation.
Lancet 9:580
3. lagannath S, Oicke KA, Armitage JO, Cabanillas F, Horwitz LJ,
Vellekoop L, Zander AR, Spitzer G (1986) High-dose cyclophosphamide,
carmustine, and etoposide and autologous bone marrow transplantation
for relapsed Hodgkin's disease. Ann Intern Med 104:163-168
4. lagannath S, Armitage 10, Oicke KA, Tucker SL,Velasquez WS, Smith
K,Vaughan WP, Kessinger A, Horwitz LJ, Hagemeister FB, Cabanillas
F Spitzer G (1989) Prognostic factors for response and survival
after high-dose cyclophosphamide, carmustine, and etoposide with
autologous bone marrow transplantation for relapsed Hodgkin's disease.
J Clin Oncol 7:179-185
5. Sheridan WP, Morstyn G, WolfM, Oodds A, Lusk J, Maher O, Layton
JE, Green MO, Souza L, Fox RM (1989) Granulocyte colony-stimulating
factor and neutrophil recovery after high-dose chemotherapy and
autologous bone marrow transplantation. Lancet 2:891-895
6. Spitzer G, Hester J ( 1991) What advantages are there to using
peripheral blood collection over autologous bone marrow in modifying
the toxicity of high-dose therapy? In: Henon P,Wunder E (eds) Peripheral
blood stem cell atuografts. Springer, Berlin Heidelberg New York
7. Spitzer G, Oicke KA, Litam .J, Verma OS, Zander AR, Lanzotti
V, Valdivieso M, McCredie KB, Samuels M (1980) High dose combination
chemotherapy with autologous bone marrow transplantation in adult
solid tumor. Cancer 45:3075-3085
8. Spitzer G , Verma OS, Fisher R, Zander AR, Vellekoop L, Litam
J, McCredie KB, Oicke KA (1980) The myeloid progenitor cell- its
value in predicting hematopoietic recovery after autologous bone
marrow transplantation. Blood 55:317-323
9. Spitzer G, Ventura G, Jagannath S, Fogel B, Taylor K, Huan S,
Ounphy F, Oicke K, Souza L, Yau J, LeMaistre CF and Spinolo J(1990)
Use of recombinant human hematopoietic growth factors and autologous
bone marrow transplantation to attenuate the neutropenic trough
of high-dose therapy. Int J Cell Cloning 8:249-261
10. Taylor K, lagannath S, Spitzer G, Spinola JA, Tucker SL, Fobel
B, Cabanillas F, Hagemeister FB, Souza LM (1989) Recombinant human
granulocyte colony-stimulating factor hastens granulocyte recovery
after high-dose chemotherapy and autologous bone marrow transplantation
in Hodgkin's disease. J Clin Oncol 7: 1791-1799
11. To LB, Oyson PG, Branford AL, Russell JA, Haylock OM, Ho JQK,
Kimber RJ, luttner CA ( 1987) Peripheral blood stem cells collected
in very early remission produce rapid and sustained autologous hemopoietic
reconstitution in acute non-Iymphoblastic leukemia. Bone Marrow
Transplant 2: 103-101
|