In: Zander AR, Barlogie B (eds) Autologus Bone Marrow Transplantation for Hodgkin`s Diseaes, Non-Hodgkin`s Lymphoma and Multiple Myeloma, Springer-Verlag, Berlin Heidelberg New York London, |
|
Introduction A significant proportion of patients who develop Hodgkin's disease (HD) or aggressive non-Hodgkin's lymphoma (NHL), can be cured with conventional therapy. However, patients who have primary refractory disease or who relapse after systemic chemotherapy are only rarely cured with any form of salvage therapy [1,2]. High-dose chemoradiotherapy followed by autologous stem cell transplantation has improved the outlook for those patients and in select groups may yield a 35% -40% chance of cure [3-5]. While autologous stem cell transplantation is associated with an increased morbidity and mortality, patient selection using clinical criteria with prognostic value such as sensitivity of the tumor to salvage therapy, tumor burden at entry, and overall performance status may result in lower rates of toxicity. In addition, comparisons between trials using different prospective regimens may identify ones that are relatively less toxic. Sixty patients who underwent autologous transplantation for relapsed or refractory HD or NHL are described in this report and analyzed retrospectively to determine whether their disease status on entry could predict the outcome from transplantation. Since more than 90% of these patients received an identical regimen consisting of carmustine, etoposide, cytosine arabinoside, and cyclophosphamide as preparative chemotherapy, the efficacy and toxicity of this regimen is also retrospectively evaluated.
Between November 1988 and April 1991, 60 patients with relapsed
or refractory HD or aggressive NHL underwent marrow or peripheral
stem cell transplants at the University of Rochester Medical Center,
Rochester, New York. Most patients were treated pretransplant with
one or more courses of dexamethasone, cytosine arabinoside, and
cisplatinum (OHAP) [6]. Patients included 21 women and 39 men; these
underwent marrow transplant (51) or peripheral stem cell transplant
(9) at a median age of 39 years (range 9-64). Thirty patients had
HO and 30 had aggressive NHL. Based on pre-transplant clinical and
radiological evaluation, 35 patients (18 HD, 17 NHL) were defined
as having minimal disease (all disease areas <- 2 cm), and 25 patients
(12 HO, 13 NHL) were defined as having bulky disease areas (at least
one area >2 cm). Of the 60 patients in this series, 55 received
the BEAC conditioning regimen: carmustine (300 mg/m²) on day -7;
etoposide (lOO mg/m² bid) on days -6, -5, -4, -3; cytosine arabinoside
(lOO mg/m² q 12 h) on days -6, -5, -4, -3, and cyclophosphamide
(35 fig/kg) on days -6, -5, -4, -3. Five patients received total
body irradiation (TBI). On day 0, 51 patients received unpurged
autologous marrow, with a median of 1.4 times 108 NBC/kg, and 9
patients received autologous blood stem cells, with a median of
7.5 time 108 NBC/kg. Survival curves are based on the actual survival.
An event is defined as death from any cause, disease relapse, or
progression. 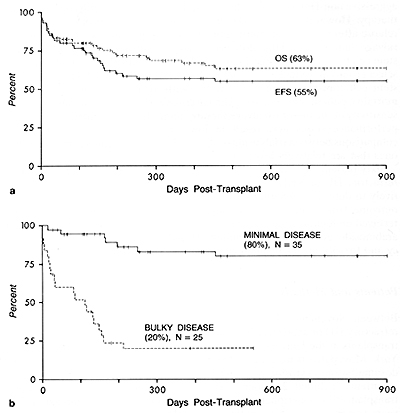
Survival 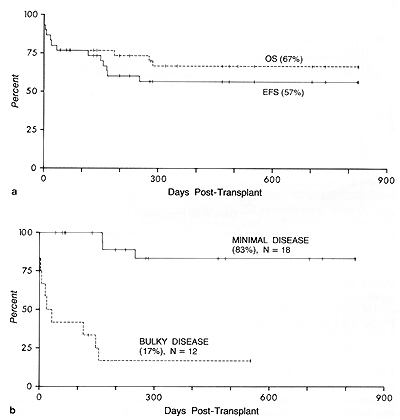 Fig. 2a, b. Patients with Hodgkin's disease (n=30). a Event-free survival (EFS) and overall survival ( OS) .b Effect of pretransplant disease status on EFS 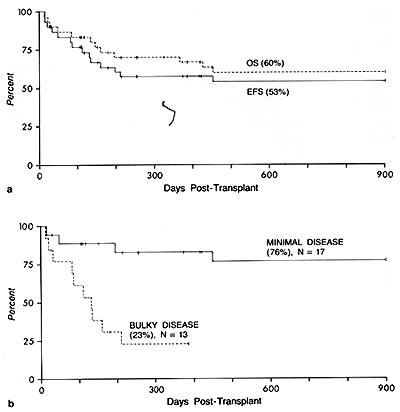 Fig. 3a, b. Patients with Hodgkin's disease (n=30). a Event-free survival (EFS) and overall survival ( OS) .b Effect of pretransplant disease status on EFS
Characteristics of Engraftment Table I. Severe or life-threatening nonhematological
toxicity (n = 60) 
It appears clear from the above data, that patients entering transplant with "bulky" disease are more likely to succumb to complications of therapy or suffer early relapse. In contrast, those patients with minimal disease had a very low overall mortality as well as a low early relapse rate. It is likely that a significant proportion of patients who entered the study with minimal disease will be long-term survivors. The BEAC chemotherapy regimen was very well tolerated in this patient population, but was associated with a significant risk of cardiopulmonary toxicity in those patients entering with "bulky" disease. Only 3% of patients died from sepsis (both due to fungal etiologies) , and there was no severe (ECOG grade 3 or 4) hepatic toxicity or mucositis. Additional follow-up is clearly needed as it is obvious that with time these results cannot be maintained. Nevertheless, at this stage of the trial, the results compare very favorably with other published reports and appear to confirm the benefit that autologous stem cell transplantation may confer on patients with relapsed or refractory Hodgkin's disease or non-Hodgkin's lymphoma. Nonetheless, it is clear that additional approaches are needed to improve efficacy and reduce the toxicity of autotransplantation for patients with bulky disease at the time of transplantation.
1. Rosenberg SA (1987) Autologous bone marrow transplant in non-Hodgkin's
lymphoma. N Engl J Med 316:1541-1542 |